December 2024 Edition — The Food Archive
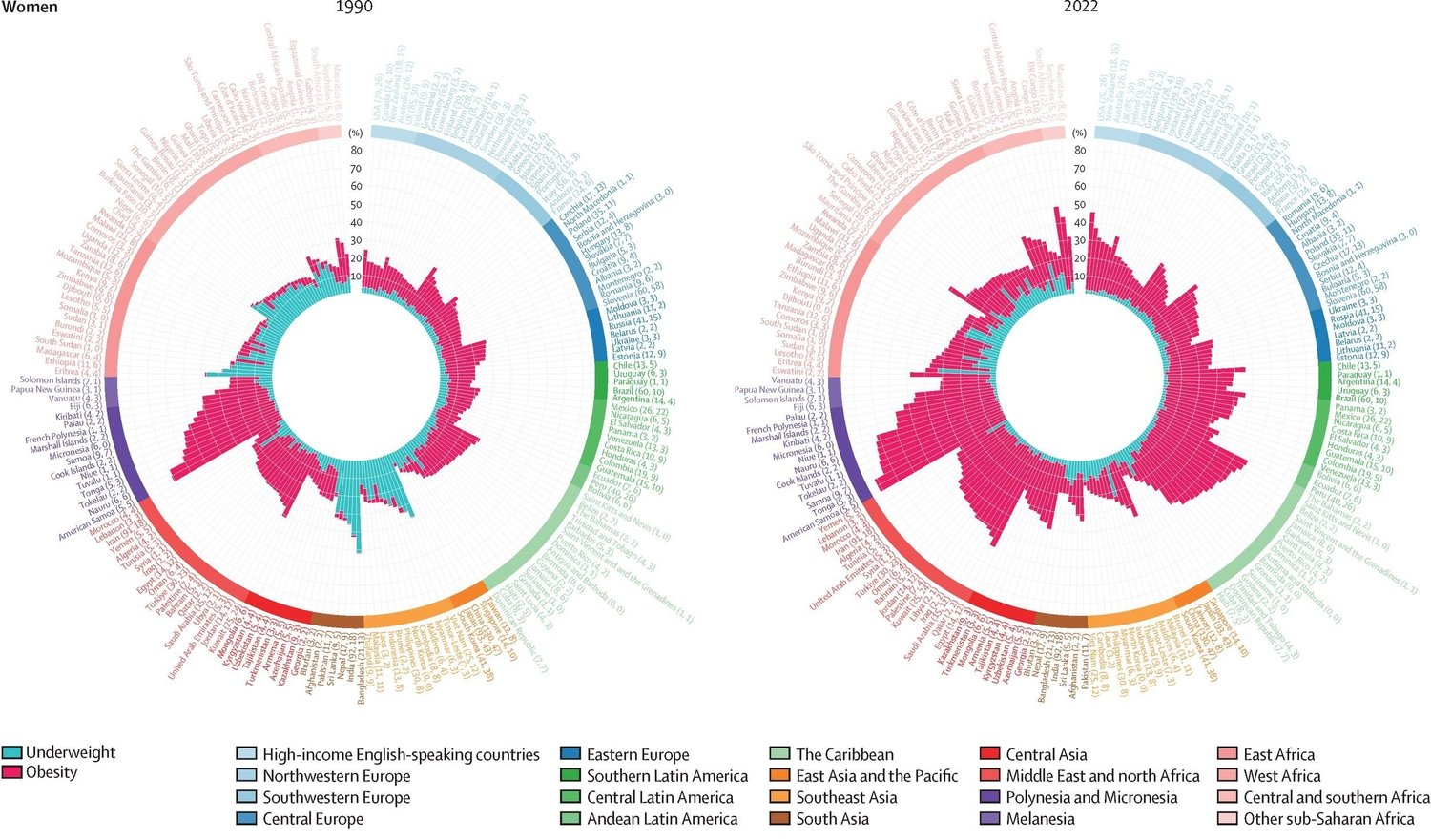
Another paper just released, again in the Lancet, showed in the United States, between 1990 and 2021, the percentage change in the prevalence of obesity in adults was 123.6% in men and 99.% in women. They forecast that by 2050 if current trends continue, the total number of adults with overweight and obesity will reach 213 million. And I am not even reporting on teen prevalence. Wowsa. Yet, JAMA just published results that found that the prevalence of BMI and obesity in the United States decreased in 2023 for the first time in over a decade. Some pontificate it is because of the GLP1 inhibitors, others because of COVID-related deaths (obesity being a heightened risk factor for morbidity and mortality associated with COVID).
The difference could be that the Lancet paper by the Global Burden of Disease 2021 US Obesity Forecasting Collaborators didn’t investigate trends beyond 2021. In contrast, the JAMA authors showed a decline in 2023 specifically. Also, we don’t know the future of the GLP-1s. Currently, they are cost-prohibitive for many living in the United States and, moreover, the world. One report estimated that if half of U.S. adults with obesity took these drugs, it could cost the healthcare system $411 billion per year. The inequities in who has access to these drugs are staggering.
These medications certainly help people lose weight, with various studies showing reductions in body weight somewhere between 10-25%, as well as other benefits for those struggling with diabetes and cardiovascular disease, to name a few. I worry that we still know so little about obesity, its drivers, and the potential ramifications of medicalizing the challenge into one silver-bullet solution. I also fear that the scale-up of these drugs gets food systems and industry “off the hook.” Why stop making ultra-processed foods and ensuring food environments are healthy for people when they can easily take these drugs? But RFK Jr is going to solve all that, right? Don’t hold your breath. I appreciated this commentary by Francesca Celletti and colleagues in JAMA on where we are at in our understanding of obesity:
“The seriousness of the crisis is now widely recognized. Yet there are many challenges that continue to hinder a successful national and global response. Perceptions and attitudes toward obesity, including the debate about whether obesity represents a risk factor or a disease, are widely divergent. Efforts to address the stigma associated with obesity have, in some cases, evolved into a narrative that obscures the importance of obesity-related morbidity and mortality. Compared with other noncommunicable diseases, there remains a lack of knowledge on the associated biological and genetic factors, and there are inconsistencies in the appreciation of the effect of obesity on other noncommunicable diseases and the overall burden of disease. There is limited evidence on long-term management interventions and their effectiveness among populations most at risk and in low-income settings in relation to issues such as access and adherence.”
Speaking of nutrition trends, the Global Burden of Disease Group published their analysis on global, regional, and national progress towards achieving the six nutrition-related Sustainable Development Goal (SDG) targets by 2030. The picture ain’t so rosy. These are their high-level results: “In 2030, we project that 94 countries will meet one of the six targets, 21 countries will meet two targets, and 89 countries will not meet any targets. We project that seven countries will meet the target for exclusive breastfeeding, 28 for child stunting, and 101 for child wasting, and no countries will meet the targets for low birthweight, child overweight, and anaemia.” Looking at current trends, the authors show that in 2021, seven countries had already met two of six targets (Georgia, Mongolia, South Korea, Peru, Rwanda, American Samoa, and Puerto Rico). What are they doing right? Case studies, anyone?
Diets heavily weigh into dietary outcomes, and as the SDGs stand, there is no target or monitoring of a dietary indicator, such as dietary diversity. SDGs. One of the juggernauts of our diets is how much animal source foods we should or could consume that benefit our health and the planet. A PNAS special feature delves into this quandary in what I think is quite a balanced set of papers showing all the angles and issues. We contributed a piece laying out the biological nutritional vulnerabilities stemming from high micronutrient needs per calorie among infants and young children, women of reproductive age, pregnant and lactating women, and older adults, particularly older women, and the importance of nutrient-dense foods coming from both plant and animal-source foods. Speaking of nutrient-dense foods, some colleagues from the Blue Foods Assessment published a paper in the Environmental Research Letters that assessed nutrition-sensitive climate risk to five essential micronutrients across production systems. By mid-century (2041–2060), we estimate that 75% of calcium, 30% of folate, 39% of iron, 68% of vitamin A, and 79% of vitamin B12 produced in primary food products will face frequent climate extremes globally. Nearly 50 countries are projected to face high domestic climate risk for two or more micronutrients during this period. Check out the figure below.











Post Comment